Arthritis Research
How to enjoy sex with arthritis
Will arthritis affect my sex life?
There are a number of ways that
arthritis can affect your sex life:
- Arthritis can affect your mood and general wellbeing which, in turn, can affect your sex drive.
- Swollen joints can affect your self-confidence and make you feel less attractive.
- Fatigue associated with arthritis can reduce your sexual desire. Your healthcare team can advise you on ways of managing fatigue and conserving energy – more information is available in our fatigue section.
- Painful joints may make it more difficult to move into a position you’re used to.
- Arthritis sometimes leads to a dry vagina, which may make sex uncomfortable. Water-based lubricating gels such as KY Jelly or Aquagel may help. You can get these on prescription or from a pharmacy, supermarket or online. Oil-based lubricants such as Vaseline or baby oil may irritate your skin or damage condoms. If you're going through the menopause this can cause vaginal dryness – discuss this with your doctor as treatment is available.
Sex isn't equally important to all couples, but if it has been important to you and your partner then you should try to find ways to meet both your needs.
Will drugs affect my sex life?
Most drugs commonly used to treat
arthritis are unlikely to affect your sex life, although
steroids can sometimes reduce sexual desire or cause temporary impotence. You should discuss your medications with your doctor if you think they may be affecting you in this way.
Drugs commonly used to treat arthritis shouldn’t reduce the effectiveness of the contraceptive pill, but check with your doctor if you’re not sure.
Talk to your partner
It is not uncommon for people with a long-term illness to have low self-image, which can lessen your desire to have sex and have an impact on intimacy. If you feel self-conscious about swollen joints or other signs of arthritis, tell your partner. They may not be aware of how you feel and may have their own fears and concerns they want to talk about.
Worrying in silence can make matters worse. Talking, whether it's with your partner, your rheumatology team, or a counsellor, can help put your mind at rest.
Change your routine
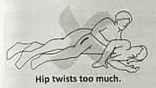
Most people with arthritis find that their pain can vary from day to day, so you may want to make the most of opportunities on your better days. If you experiment with
different positions, you should be able to find some that are more comfortable for your joints.
Sometimes, making little changes can make a big difference. In the same way that getting your medication right can take trial and error, changing your routine can make it easier to have a fulfilling sex life.
For example, if you find that you're too exhausted then and your pain is worse, try making love in the morning or early evening. Spontaneity is all well and good – but like many things when you have arthritis, you need to plan ahead.
Taking painkillers in the lead up to sex can help. If your joints and muscles are achy, have a warm bath to help you to relax or ask your partner to give you a massage. Before you get started, make sure you have pillows or bean bags for support to hand.
Best sex positions
Durex sex and relationship expert
Susan Quilliam advises a side-by-side position, where you both lie facing and with her outer leg raised up and over his waist, means that your bodies are supported.
"Unlike the missionary position where she's underneath, or 'woman on top', it means that neither of you is taking the weight of the other.
"It's also a gentle position, that doesn't take much exertion or acrobatics, and being face-to-face makes it very intimate. The alternative side-by-side position is 'spooning', where she lies in front, he lies behind her and curled round, penetrating. This may not be as romantic but does mean that either of you can reach down and stimulate her clitoris."
Best sexual positions and tips to try
If you one or both of you has had a hip replacement or has problems with kneeling or lying face down, try a standing position. Both partners stand, with the woman resting on furniture at a comfortable height to provide support and balance, while the man enters from behind.
If you're a woman who can't bend your hips or straighten your knees, try lying on your back on the edge of the bed. Your partner then kneels on the floor and enters from in front.
Arthritis Research UK has a list of positions -
illustrated with line drawings - suggesting the best positions for various problems.
When dryness is a problem
Arthritis can sometimes lead to a dry vagina, which may make sex uncomfortable. "Added to that, a woman's ability to lubricate drops naturally after the menopause, particularly if she is not using hormonal supplements," says Susan.
If dryness is a problem, Susan suggests using a water-based lubricating gel.
"I'd recommend
Durex Play O which not only lubricates but also enhances orgasm. Also, make sure that foreplay is long and arousing to encourage natural lubrication. Plus, keep having sex for as long as you want it - so you don't 'lose it' because you don't 'use it', whether that's with partner sex or pleasuring yourself."
Think beyond intercourse
Sexual fulfilment doesn't have to mean penetration – using sex toys can be a way to enjoy sexual satisfaction and promote intimacy. Most toys can be bought online and delivered discreetly (in plain packaging). Even Boots and some supermarkets now have a range of vibrators.
Susan says: "If you're not used to using one, I would recommend a
compact vibrator for clitoral stimulation. Because it's smaller, it can be easier to introduce into your love making."
There will be times when you just don't have the energy or the pain is too much. Try not to place too much pressure on yourself or your partner. Keep talking and sharing your feelings. Many couples find that they become closer by discussing things openly and that their relationship is stronger as a result.
Will we be able to have a baby?
There’s no reason why arthritis should prevent you from having children, but you should discuss it with your doctor before trying for a baby for the following reasons:
- Some drugs, such as sulfasalazine, can temporarily reduce the sperm count in men.
- Some studies suggest that non-steroidal anti-inflammatory drugs (NSAIDs) may increase the risk of miscarriage if taken around the time of conception.
- Methotrexate and leflunomide can be harmful to an unborn child so need to be stopped at least three months (some doctors recommend six months) before trying to conceive. For leflunomide, you may be able to have a special 'washout' treatment to remove the drug from your body more quickly. It’s important to discuss contraception with a health professional if you're taking one of these drugs.
- Women with lupus and/or antiphospholipid syndrome may have a greater risk of miscarriage, so your condition and the pregnancy may need to be more closely monitored than usual. If you're thinking of having a baby it's best to discuss this with your rheumatology team beforehand.
- Some drugs may pass into the breast milk and could be harmful to your baby so it’s best to discuss with your doctor beforehand which drugs you can safely use if you wish to breastfeed.
Women with arthritis may find they have more discomfort in the back, hips or knees during pregnancy because of their increasing weight. Women with lupus may have flare-ups of their symptoms during pregnancy, but women with
rheumatoid arthritis may find their symptoms ease while they're pregnant.
Childbirth can aggravate pain in these joints, but most women can find a position that allows them to give birth naturally.
 United States
United States