What you may see and experience in the hospital
Dressings
Immediately following knee replacement surgery, your doctor will most likely send you to recovery with a leg bandage that looks like the photo below. The wraps provide compression that helps reduce swelling and discomfort. It is usually removed after a few days.
Hip replacement surgical wounds are usually covered with a single large dressing such as the AQUACEL® Ag SURGICAL cover dressing you see in the photo to the left. This special type of dressing is a silver-impregnated antimicrobial product designed to be left in place for 7 days or as directed by surgeon. It has a waterproof barrier that permits showering with no additional covering required. This type of dressing is widely used and popular with both surgeons and patients.
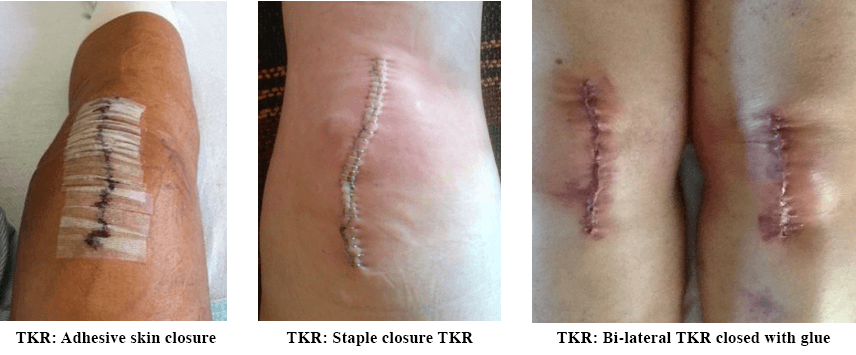
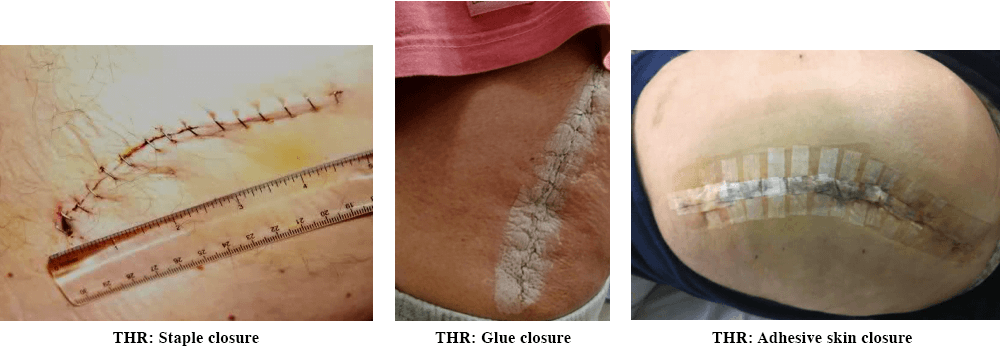
If you’re staying overnight or a few days in the hospital before going home, your nurses may do one or more dressing changes on your wound. Here is what to expect your wound to look like once the dressing is removed. But it is also quite possible your original dressing will remain in place for a week or more, depending on what your surgeon prefers.
Wound Drainage
While extensive fluid buildup can be a sign of serious complications following surgery, some fluid drainage from your incision is part of the normal healing process. Your wound should be at least partially moist. Many factors influence drainage such as trauma to the site, presence of bacteria, damage to capillaries as well as increased levels of inflammation and infection. You should expect to see some drainage immediately following your surgery. Your medical team will keep a watchful eye on your incision to ensure you stay within a normal range.
Doctors use a scale to determine whether wound drainage is becoming a problem. If a dressing is 25% saturated with moisture (blood or fluid), drainage is considered minimal. Saturation between 25% and 75% is considered to be moderate and still not a concern. It’s only when drainage exceeds the 75% saturation level that the situation can potentially have a negative impact on proper wound healing.
In addition to the amount of fluid, consideration is also given to its color and consistency. There are four different types of drainage you may experience:

• Serous – a clean, watery discharge that is usually considered normal
• Sanguinous – dark red color normally associated with broken capillaries
• Serosanguinous – thin, pink-colored discharge that is usually part of
a normal wound recovery
• Purulent – a generally thick green or yellow discharge usually indicative
of infection
If the drainage is determined to be a problem, your surgeon has a number of ways to manage it. The most basic treatment is the use of dressings. There is a wide variety of types designed for either absorption or regulating moisture content of the wound area. Compression can be added to control drainage flow. There are also several vacuum-assisted options which not only can remove drainage, but also any bacteria or other toxic debris.
Wound Drain
You may have a wound drain similar to the one pictured installed near your incision while you are in surgery. Drains are used to quickly remove free blood from the surgical site. This has been a very common practice for many years, but some fairly recent studies (https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5115035/ and https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3934272/ ) showed no significant advantage and at some point, using drains may be discontinued. If you do have a wound drain, it usually will be removed after a day or two and you normally shouldn’t have to deal with it at home.
Wound Vacuum – Negative-Pressure Wound Therapy (NPWT)
Because joint replacement surgery requires separation of tissue planes and extensive tissue manipulation, it is normal for some amount of fluid to collect within the surgical wound. If a patient is at risk for potentially high levels of fluid buildup, wound healing can be impacted as the fluid can impede normal blood flow and can lead to the formation of dense fibrous tissue. Prior to NPWT, surgeons were limited to compression dressings and wound drains to deal with the problem of excess fluid buildup.
Surgeons now may opt to use Negative-Pressure Wound Therapy (NPWT), commonly referred to as a wound vacuum or wound vac. An example of this technology is pictured below. The single-use PREVENA™ Incision Management System protects the incision from external contamination, helps hold incision edges together, removes fluid and infection materials, and delivers continuous negative pressure for up to seven days. Although there has not been a lot of testing done to definitively point to the benefits of a wound vac in all cases following joint replacement surgery, this device can enhance wound healing and help prevent site infections as well as remove fluid and stabilize the wound environment. And, while not necessary for everyone, clinical evidence appears to support the use of a wound vac for patients who have higher risk for excessive post-operative drainage. As more clinical trials are completed, use of wound vacs may soon be incorporated into clinical guidelines as a means to help prevent periprosthetic joint infections.
And Then It’s Time for Discharge
Once you’re ready to go home from the hospital, you can expect to have wound care instructions provided for you as part of your discharge instructions. The hospital social worker should arrange for you to have at least an initial visit by a Home Health Nurse. Be sure to have the discharge nurse clarify anything that you don’t completely understand. It will be helpful to have a friend or family member there during the discharge process to be sure everything is discussed.