Management of pain
A. D. Toms, V. Mandalia, R. Haigh, B. Hopwood From the Royal Devon and Exeter Hospital, Exeter, England: J Bone Joint Surg [Br] 2009;91-B:143-50.
(LINK is no longer available)
The management of painful TKR requires a multidisciplinary approach involving surgeons, physiotherapists, and pain management teams, particularly if there is an element of neuropathic pain. The patient’s general practitioner should also be involved. It is generally accepted that unrelieved acute severe pain can exacerbate the patient’s pre-operative tendency for anxiety, depression, hostility and pre-occupation with health.
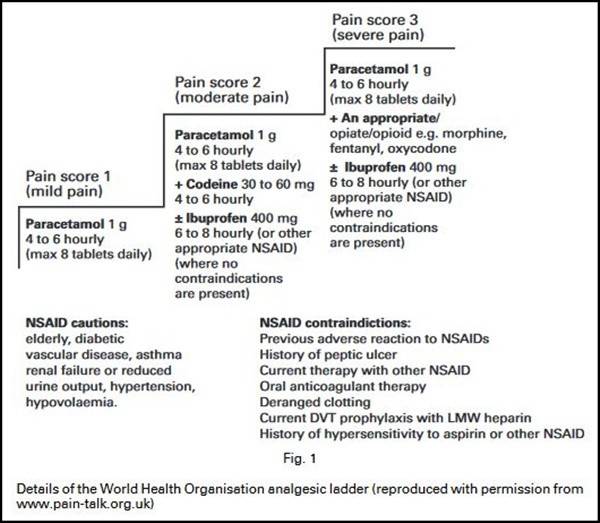
Many patients report low pain scores in the first three months after TKR, but in some the pain fails to improve and actually increases as time passes. This often correlates with the cessation of regular analgesia by the patient who may feel that it is not required for such a long period after their operation. At this stage there is often no input from physiotherapists and the increase in pain can lead to a reduction in the range of movement, with subsequent stiffness and increased sensitivity around the joint. Patients should be encouraged to take analgesics regularly, and these should be prescribed according to the World Health Organisation (WHO) analgesic ladder. Reluctance to take oral medication can be overcome by the prescription of sustained-release opiates including patches. Fentanyl and Butrans are commonly used opiate patches and as such should be managed in the same way as any opiate used for a non-malignant cause according to the guidelines laid down by the British Pain Society. Patients need to be aware of and should have an explanation of the side-effects and the implications of opiate analgesia. Occasionally, the pain may not respond to one form of opiate, and another formulation should be tried.
Management of neuropathic pain
Clinical assessment should also focus on identifying any specific elements of neuropathic pain, which include dysaesthesia (abnormal sensation, painful or not, including numbness or hypo-aesthesia), allodynia (pain associated with a normally non-noxious stimulus), hyperalgesia (increased response to a normally mildly noxious stimulus) and spontaneous pain.
Discrete areas of local dysaesthesia may respond to the use of topical applications such as capsaicin cream or 5% lignocaine plasters. Patients are more at ease with the concept of applying topical analgesics rather than having systemic medication. Regular massage of the scar or the painful site may help desensitisation in its own right and thereby prevent neglect of the joint and subsequent stiffness. Capsaicin cream is an effective agent and acts by promoting the release of substance P from peripheral nerve endings, thereby decreasing sensitisation. Excessive burning or rashes may occur, but the irritant effect usually diminishes after repeated use. The application of 5% lignocaine plasters to the painful area for periods of 12 hours is often better tolerated and can help by providing a physical barrier. A therapeutic trial of two weeks is sufficient to judge whether to continue with this form of therapy. If, however, the first line of treatment is unsuccessful it may be necessary to progress to a trial of oral medication.
Management of a painful neuroma
Patients with symptomatic neuromas around the knee who have tried conservative therapy for at least six months may be helped by resection of the neuroma.10 A positive preoperative response to local anaesthetic blocks or patches is crucial for identifying those who will benefit from surgery. The most common surgical method is selective denervation of the nerve. A satisfaction rate of up to 86% has been reported. Patients should be warned of a high incidence of minor potential complications which can occur in up to 40% as well as of hypersensitivity that can result from collateral sprouting from the normal adjacent nerve. This is a response of the uninjured nerve to the nerve-growth factor released by Schwann cells in the divided distal degenerated nerve fibres. This problem is self-limiting and gentle desensitisation resolves the issue over three to six weeks.
Management of complex regional pain syndrome #CRPS
This can develop after TKR, although the full-blown syndrome is uncommon. The only prospective study examining this in some detail reported a prevalence of 21% at one, 13% at three and 12.7% at six months after operation. Psychological predictors such as pain, anxiety and depression were also assessed. Pre-operative pain and distress
were found to be risk factors for the development of such symptoms after TKR. Recognition of complex regional pain syndrome relies on the identification of diffuse skin, joint and muscle pain, sensory disturbances and neuropathic pain.
Infection
Variables which affect decision-making in the treatment of the infected TKR include whether the infection is superficial or deep, the duration since surgery, host factors, the condition of the soft tissue around the knee and the underlying organism. The goals of treatment include the eradication of the infection, the alleviation of pain and the recovery of function. Treatment options include antibiotic suppression, arthroscopic or open debridement, one- or two-stage revision arthroplasty, arthrodesis and amputation in chronic unremitting infection. A full review of this topic is beyond the scope of this article and we refer the reader to recent publications covering this in detail.
Instability
Patients with an unstable TKR often have associated pain because of the abnormal stresses placed on the knee and the soft-tissue envelope. It is important to ascertain the true nature of instability because those with quadriceps weakness,
flexion contracture or patellofemoral maltracking and pain may describe their symptoms as instability. After TKR instability may occur in flexion, extension, mid-flexion, globally and in hyperextension. Instability in the early post-operative period may be due to uncorrected pre-operative ligamentous imbalance, improper intra-operative ligamentous balancing, mismatch of the flexion-extension gap, iatrogenic injury to the ligaments during surgery or pre-existing neuromuscular pathology. However, late instability can occur secondary to malalignment leading to progressive stretching of the ligaments, wear of polyethylene, loosening of the component and collapse.
Problems of the extensor mechanism
Complications involving the extensor mechanism and the patellofemoral joint are common causes of pain and an unsatisfactory outcome after TKR. These include patellofemoral maltracking and instability, disruption of the extensor mechanism, the patellar clunk syndrome, peripatellar adhesions, wear of polyethylene and osteonecrosis.
Patellofemoral instability.
In the past an incidence of patellar subluxation and/or dislocation of 10% to 35% has been reported after TKR. However, with improved awareness of the intricacies of patellar tracking, newer prosthetic designs and sided components the incidence has fallen to < 1%. Patellofemoral instability can be secondary to malrotation of the implant, ‘overstuffing’ of the patellofemoral joint, softtissue imbalance or asymmetrical resection of the patella. Conservative management includes strengthening of vastus medialis obliquus and bracing, but is not generally useful because the instability is generally secondary to a structural problem. The mainstay of treatment is therefore surgical.
Malrotation of the tibial or femoral components.
This is difficult to address without revision of one or both of the components. However, if the components are in the correct rotational alignment, a lateral retinacular release may be used to improve the patellofemoral biomechanics.
However, this is not a benign procedure and the potential complications, particularly problems with wound healing, avascular necrosis of the patella, patellar fracture,increased post-operative pain, swelling and a subsequent slower rehabilitation should be borne in mind.
Rupture of the patellar tendon.
This is an uncommon complication after TKR with a reported incidence of 0.17% over a period of 12 years.
Quadriceps tendon rupture.
This is a rare complication after a TKR with one study reporting an incidence of 1.1% in a series of 281 TKRs. The exact aetiology is often not clear, but possible risk factors include quadriceps turndown, over-resection of the patella with damage to the tendon, manipulation or an extensive lateral release. It requires direct repair depending on the level of the tear and the volume and the quality of the patella.
Peri-prosthetic fracture of the patella
The incidence of post-operative fracture of the patella is reported to be between 1% and 2%.35,38,50 Predisposing factors include a lateral release, excessive resection of bone, single peg fixation, maltracking of the patella and a malpositioned implant. The management of a fracture after TKR depends upon its location and pattern, the integrity of the extensor mechanism, the stability of the implant and the quality of the bone.
Stiffness
The incidence and definition of post-operative stiffness after a TKR are not well described in the literature and vary
widely between 3% and 60%. The stiff knee is often painful and leads to functional limitation in the activities of daily living. Stiffness as a term is a common presenting complaint used by such patients, but it is vital to clarify the symptoms and to define properly what the patient is limited by or unhappy about. There are many contributing factors, but stiffness can be associated with a poor pre-operative range of movement, previous knee surgery, infection, technical errors (component malpositioning, oversizing of components, ‘overstuffing’ of the patellofemoral joint, ligament imbalancing, elevation of the joint line), complex regional pain syndrome, or severe post-operative pain preventing appropriate rehabilitation.
Post-operative control of pain after TKR is of paramount importance. Uncontrolled pain often leads to a reduced range of movement and adhesions in the suprapatellar pouch. It is suggested that with proper control of pain, the incidence of manipulation for stiffness may be decreased from 9% to less than 1%, although, as stated, stiffness is rarely clearly defined.
The options for treatment for the stiff knee include intense physiotherapy, manipulation of the knee under anaesthesia (MUA), arthroscopic or open arthrolysis and finally a revision procedure. This should only be performed if stiffness does not improve after intense physiotherapy. Unfortunately, there is no strong agreement on either the optimum timing of MUA or on the key indications for it. Yercan et suggested that if patients with a good preoperative range of movement had no progression or regression in range of movement after wound healing, there was no need to delay MUA. However, Esler et suggested that MUA up to four months after TKR can result in a sustained improvement in flexion. We believe that MUA at two to three weeks is too early unless the patient has had a large haematoma or a medical condition which has prevented normal postoperative rehabilitation. In our opinion the key indications for a MUA is a failure to regain the pre-operative range of movement at six weeks post-operatively, failure to progress or regression after a good initial attempt at rehabilitation.
MUA is not without risks such as fracture, rupture of the patellar tendon, wound breakdown and haemarthrosis, and the rehabilitation after manipulation is critical to the success of the procedure. Manipulation should be followed by good analgesic cover with in-patient physiotherapy providing support and encouragement. Arthroscopic release may have a role at three to six months after TKR in a moderately stiff knee which is otherwise well-aligned and well-balanced in a well-motivated patient. Associated release of the posterior cruciate ligament (PCL) in particular can be successful in a stiff knee with a cruciate-retaining TKR.
Impingement syndromes
The diagnosis and assessment of these conditions have been discussed.
Impingement of the popliteus tendon
The popliteus tendon syndrome is difficult to diagnose and can be the cause of considerable discomfort after TKR. It can be treated effectively by arthroscopic release of the tendon from its femoral insertion.
Fabellar impingement (fabella - a small sesamoid bone - sesamoid as in sesame seed because they are often similarly shaped!)

This should be considered in patients with discrete posterolateral pain after TKR and with a large fabella seen on radiographs. Pain is usually activity-related and is due to impingement of the fabella on the femoral or tibial component. The diagnosis can be further confirmed by dynamic ultrasonography. The patients generally respond well to excision of the fabella.
Patellar clunk syndrome
This is a well-recognised complication of the older designs of the posterior-stabilised TKR with a reported incidence of up to 3.5%.
Patients with soft-tissue impingement under the patella can be divided into three main groups as follows:
1) patellar clunk syndrome, an isolated fibrous nodule located in the suprapatellar region without other fibrous tissues causing impingement;
2) impinging hypertrophic synovitis, generalised hypertrophic synovitis with no fibrous nodule; and
3) the combination of types I and II.
Most patients with an established clunk syndrome require surgery and excellent results have been reported with arthroscopic resection through a superolateral portal.
Recurrent haemarthrosis
In the absence of a bleeding disorder, the most common underlying pathology for recurrent haemarthrosis is impingement of the proliferative synovium with fibrosis and deposition of haemosiderin. The condition can be treated conservatively, but if this fails, surgical treatment is usually successful. This involves an arthroscopic or open synovectomy and surgical embolisation in cases in which an obvious source of bleeding can be identified. Open synovectomy offers the advantage of better access and allows a more thorough debridement compared with arthroscopic synovectomy, especially if there is associated stiffness of the knee.
The role of arthroscopy in painful TKR
Most studies examining the role of arthroscopy in painful TKR have involved relatively few patients and have failed to report any objective outcome measures. However, certain types of pathology can be dealt with effectively by an arthroscopic intervention. Klinger et al reviewed the results of arthroscopy in 27 patients with TKR and summarised the literature from 44 studies between 1966 and 2002. Arthroscopy was found to be useful in the treatment of patients with soft-tissue impingement (patellar clunk syndrome, popliteus tendon impingement, PCL impingement, impingement of a retained meniscus or pseudomeniscus), arthrofibrosis, loose body (e.g. PMMA fragments) and acute infection.
It is recommended that patients undergoing arthroscopy should receive prophylactic intravenous antibiotics for 24 to 48 hours and special care must be taken to avoid scratching or gouging the implants with the arthroscope, since this has obvious implications regarding the generation of wear debris.
Unexplained pain after TKR
A review based on the England and Wales National Joint Registry reported that at more than one year after TKR, 18.2% of patients were not satisfied with the outcome, usually because of pain.85 It is not clear as to how many of these patients had an explanation for their pain. Brander et al in a prospective study of 116 patients found that 13.1% had unexplained pain one year after surgery. However, after conservative treatment, nearly all of these patients were satisfied at the follow-up at five years. Elson and Brenkel88 in a series of 622 TKRs, found that 4% of patients had unexplained pain of whom 55.5% went on to show an improvement without intervention. The results of revision operations in these patients are at best unpredictable and should therefore be viewed with caution.
A. D. Toms, V. Mandalia, R. Haigh, B. Hopwood From the Royal Devon and Exeter Hospital, Exeter, England: J Bone Joint Surg [Br] 2009;91-B:143-50.
(LINK is no longer available)
The management of painful TKR requires a multidisciplinary approach involving surgeons, physiotherapists, and pain management teams, particularly if there is an element of neuropathic pain. The patient’s general practitioner should also be involved. It is generally accepted that unrelieved acute severe pain can exacerbate the patient’s pre-operative tendency for anxiety, depression, hostility and pre-occupation with health.
Many patients report low pain scores in the first three months after TKR, but in some the pain fails to improve and actually increases as time passes. This often correlates with the cessation of regular analgesia by the patient who may feel that it is not required for such a long period after their operation. At this stage there is often no input from physiotherapists and the increase in pain can lead to a reduction in the range of movement, with subsequent stiffness and increased sensitivity around the joint. Patients should be encouraged to take analgesics regularly, and these should be prescribed according to the World Health Organisation (WHO) analgesic ladder. Reluctance to take oral medication can be overcome by the prescription of sustained-release opiates including patches. Fentanyl and Butrans are commonly used opiate patches and as such should be managed in the same way as any opiate used for a non-malignant cause according to the guidelines laid down by the British Pain Society. Patients need to be aware of and should have an explanation of the side-effects and the implications of opiate analgesia. Occasionally, the pain may not respond to one form of opiate, and another formulation should be tried.
Management of neuropathic pain
Clinical assessment should also focus on identifying any specific elements of neuropathic pain, which include dysaesthesia (abnormal sensation, painful or not, including numbness or hypo-aesthesia), allodynia (pain associated with a normally non-noxious stimulus), hyperalgesia (increased response to a normally mildly noxious stimulus) and spontaneous pain.
Discrete areas of local dysaesthesia may respond to the use of topical applications such as capsaicin cream or 5% lignocaine plasters. Patients are more at ease with the concept of applying topical analgesics rather than having systemic medication. Regular massage of the scar or the painful site may help desensitisation in its own right and thereby prevent neglect of the joint and subsequent stiffness. Capsaicin cream is an effective agent and acts by promoting the release of substance P from peripheral nerve endings, thereby decreasing sensitisation. Excessive burning or rashes may occur, but the irritant effect usually diminishes after repeated use. The application of 5% lignocaine plasters to the painful area for periods of 12 hours is often better tolerated and can help by providing a physical barrier. A therapeutic trial of two weeks is sufficient to judge whether to continue with this form of therapy. If, however, the first line of treatment is unsuccessful it may be necessary to progress to a trial of oral medication.
Management of a painful neuroma
Patients with symptomatic neuromas around the knee who have tried conservative therapy for at least six months may be helped by resection of the neuroma.10 A positive preoperative response to local anaesthetic blocks or patches is crucial for identifying those who will benefit from surgery. The most common surgical method is selective denervation of the nerve. A satisfaction rate of up to 86% has been reported. Patients should be warned of a high incidence of minor potential complications which can occur in up to 40% as well as of hypersensitivity that can result from collateral sprouting from the normal adjacent nerve. This is a response of the uninjured nerve to the nerve-growth factor released by Schwann cells in the divided distal degenerated nerve fibres. This problem is self-limiting and gentle desensitisation resolves the issue over three to six weeks.
Management of complex regional pain syndrome #CRPS
This can develop after TKR, although the full-blown syndrome is uncommon. The only prospective study examining this in some detail reported a prevalence of 21% at one, 13% at three and 12.7% at six months after operation. Psychological predictors such as pain, anxiety and depression were also assessed. Pre-operative pain and distress
were found to be risk factors for the development of such symptoms after TKR. Recognition of complex regional pain syndrome relies on the identification of diffuse skin, joint and muscle pain, sensory disturbances and neuropathic pain.
Infection
Variables which affect decision-making in the treatment of the infected TKR include whether the infection is superficial or deep, the duration since surgery, host factors, the condition of the soft tissue around the knee and the underlying organism. The goals of treatment include the eradication of the infection, the alleviation of pain and the recovery of function. Treatment options include antibiotic suppression, arthroscopic or open debridement, one- or two-stage revision arthroplasty, arthrodesis and amputation in chronic unremitting infection. A full review of this topic is beyond the scope of this article and we refer the reader to recent publications covering this in detail.
Instability
Patients with an unstable TKR often have associated pain because of the abnormal stresses placed on the knee and the soft-tissue envelope. It is important to ascertain the true nature of instability because those with quadriceps weakness,
flexion contracture or patellofemoral maltracking and pain may describe their symptoms as instability. After TKR instability may occur in flexion, extension, mid-flexion, globally and in hyperextension. Instability in the early post-operative period may be due to uncorrected pre-operative ligamentous imbalance, improper intra-operative ligamentous balancing, mismatch of the flexion-extension gap, iatrogenic injury to the ligaments during surgery or pre-existing neuromuscular pathology. However, late instability can occur secondary to malalignment leading to progressive stretching of the ligaments, wear of polyethylene, loosening of the component and collapse.
Problems of the extensor mechanism
Complications involving the extensor mechanism and the patellofemoral joint are common causes of pain and an unsatisfactory outcome after TKR. These include patellofemoral maltracking and instability, disruption of the extensor mechanism, the patellar clunk syndrome, peripatellar adhesions, wear of polyethylene and osteonecrosis.
Patellofemoral instability.
In the past an incidence of patellar subluxation and/or dislocation of 10% to 35% has been reported after TKR. However, with improved awareness of the intricacies of patellar tracking, newer prosthetic designs and sided components the incidence has fallen to < 1%. Patellofemoral instability can be secondary to malrotation of the implant, ‘overstuffing’ of the patellofemoral joint, softtissue imbalance or asymmetrical resection of the patella. Conservative management includes strengthening of vastus medialis obliquus and bracing, but is not generally useful because the instability is generally secondary to a structural problem. The mainstay of treatment is therefore surgical.
Malrotation of the tibial or femoral components.
This is difficult to address without revision of one or both of the components. However, if the components are in the correct rotational alignment, a lateral retinacular release may be used to improve the patellofemoral biomechanics.
However, this is not a benign procedure and the potential complications, particularly problems with wound healing, avascular necrosis of the patella, patellar fracture,increased post-operative pain, swelling and a subsequent slower rehabilitation should be borne in mind.
Rupture of the patellar tendon.
This is an uncommon complication after TKR with a reported incidence of 0.17% over a period of 12 years.
Quadriceps tendon rupture.
This is a rare complication after a TKR with one study reporting an incidence of 1.1% in a series of 281 TKRs. The exact aetiology is often not clear, but possible risk factors include quadriceps turndown, over-resection of the patella with damage to the tendon, manipulation or an extensive lateral release. It requires direct repair depending on the level of the tear and the volume and the quality of the patella.
Peri-prosthetic fracture of the patella
The incidence of post-operative fracture of the patella is reported to be between 1% and 2%.35,38,50 Predisposing factors include a lateral release, excessive resection of bone, single peg fixation, maltracking of the patella and a malpositioned implant. The management of a fracture after TKR depends upon its location and pattern, the integrity of the extensor mechanism, the stability of the implant and the quality of the bone.
Stiffness
The incidence and definition of post-operative stiffness after a TKR are not well described in the literature and vary
widely between 3% and 60%. The stiff knee is often painful and leads to functional limitation in the activities of daily living. Stiffness as a term is a common presenting complaint used by such patients, but it is vital to clarify the symptoms and to define properly what the patient is limited by or unhappy about. There are many contributing factors, but stiffness can be associated with a poor pre-operative range of movement, previous knee surgery, infection, technical errors (component malpositioning, oversizing of components, ‘overstuffing’ of the patellofemoral joint, ligament imbalancing, elevation of the joint line), complex regional pain syndrome, or severe post-operative pain preventing appropriate rehabilitation.
Post-operative control of pain after TKR is of paramount importance. Uncontrolled pain often leads to a reduced range of movement and adhesions in the suprapatellar pouch. It is suggested that with proper control of pain, the incidence of manipulation for stiffness may be decreased from 9% to less than 1%, although, as stated, stiffness is rarely clearly defined.
The options for treatment for the stiff knee include intense physiotherapy, manipulation of the knee under anaesthesia (MUA), arthroscopic or open arthrolysis and finally a revision procedure. This should only be performed if stiffness does not improve after intense physiotherapy. Unfortunately, there is no strong agreement on either the optimum timing of MUA or on the key indications for it. Yercan et suggested that if patients with a good preoperative range of movement had no progression or regression in range of movement after wound healing, there was no need to delay MUA. However, Esler et suggested that MUA up to four months after TKR can result in a sustained improvement in flexion. We believe that MUA at two to three weeks is too early unless the patient has had a large haematoma or a medical condition which has prevented normal postoperative rehabilitation. In our opinion the key indications for a MUA is a failure to regain the pre-operative range of movement at six weeks post-operatively, failure to progress or regression after a good initial attempt at rehabilitation.
MUA is not without risks such as fracture, rupture of the patellar tendon, wound breakdown and haemarthrosis, and the rehabilitation after manipulation is critical to the success of the procedure. Manipulation should be followed by good analgesic cover with in-patient physiotherapy providing support and encouragement. Arthroscopic release may have a role at three to six months after TKR in a moderately stiff knee which is otherwise well-aligned and well-balanced in a well-motivated patient. Associated release of the posterior cruciate ligament (PCL) in particular can be successful in a stiff knee with a cruciate-retaining TKR.
Impingement syndromes
The diagnosis and assessment of these conditions have been discussed.
Impingement of the popliteus tendon
The popliteus tendon syndrome is difficult to diagnose and can be the cause of considerable discomfort after TKR. It can be treated effectively by arthroscopic release of the tendon from its femoral insertion.
Fabellar impingement (fabella - a small sesamoid bone - sesamoid as in sesame seed because they are often similarly shaped!)
This should be considered in patients with discrete posterolateral pain after TKR and with a large fabella seen on radiographs. Pain is usually activity-related and is due to impingement of the fabella on the femoral or tibial component. The diagnosis can be further confirmed by dynamic ultrasonography. The patients generally respond well to excision of the fabella.
Patellar clunk syndrome
This is a well-recognised complication of the older designs of the posterior-stabilised TKR with a reported incidence of up to 3.5%.
Patients with soft-tissue impingement under the patella can be divided into three main groups as follows:
1) patellar clunk syndrome, an isolated fibrous nodule located in the suprapatellar region without other fibrous tissues causing impingement;
2) impinging hypertrophic synovitis, generalised hypertrophic synovitis with no fibrous nodule; and
3) the combination of types I and II.
Most patients with an established clunk syndrome require surgery and excellent results have been reported with arthroscopic resection through a superolateral portal.
Recurrent haemarthrosis
In the absence of a bleeding disorder, the most common underlying pathology for recurrent haemarthrosis is impingement of the proliferative synovium with fibrosis and deposition of haemosiderin. The condition can be treated conservatively, but if this fails, surgical treatment is usually successful. This involves an arthroscopic or open synovectomy and surgical embolisation in cases in which an obvious source of bleeding can be identified. Open synovectomy offers the advantage of better access and allows a more thorough debridement compared with arthroscopic synovectomy, especially if there is associated stiffness of the knee.
The role of arthroscopy in painful TKR
Most studies examining the role of arthroscopy in painful TKR have involved relatively few patients and have failed to report any objective outcome measures. However, certain types of pathology can be dealt with effectively by an arthroscopic intervention. Klinger et al reviewed the results of arthroscopy in 27 patients with TKR and summarised the literature from 44 studies between 1966 and 2002. Arthroscopy was found to be useful in the treatment of patients with soft-tissue impingement (patellar clunk syndrome, popliteus tendon impingement, PCL impingement, impingement of a retained meniscus or pseudomeniscus), arthrofibrosis, loose body (e.g. PMMA fragments) and acute infection.
It is recommended that patients undergoing arthroscopy should receive prophylactic intravenous antibiotics for 24 to 48 hours and special care must be taken to avoid scratching or gouging the implants with the arthroscope, since this has obvious implications regarding the generation of wear debris.
Unexplained pain after TKR
A review based on the England and Wales National Joint Registry reported that at more than one year after TKR, 18.2% of patients were not satisfied with the outcome, usually because of pain.85 It is not clear as to how many of these patients had an explanation for their pain. Brander et al in a prospective study of 116 patients found that 13.1% had unexplained pain one year after surgery. However, after conservative treatment, nearly all of these patients were satisfied at the follow-up at five years. Elson and Brenkel88 in a series of 622 TKRs, found that 4% of patients had unexplained pain of whom 55.5% went on to show an improvement without intervention. The results of revision operations in these patients are at best unpredictable and should therefore be viewed with caution.



 United Kingdom
United Kingdom
