In this article:
- Overview
- Partial Knee Replacement and Unispacer Surgery
- Preparation
- During the Procedure
- After the Procedure
- Next Steps
- Risks
- Results
- When to Seek Medical Care
Overview
Knee replacement surgery is among the most remarkable of surgical innovations in orthopedic surgery. Pain relief and return of function after successful total knee replacement can often last the lifetime of the patient. Even so, the pain, rehabilitation, and recovery associated with the surgical procedure are a concern for many patients. The purpose of this article is to help familiarize you with minimally invasive knee replacement surgery, so that you can make an informed choice about the procedure.
Advances in anesthesia techniques and modern pain management methods, including the use of newer pain medications, have improved recovery following knee replacement surgery. With shorter hospital stays and an earlier return to work and daily activities, any strategy to accelerate recovery after knee replacement surgery and make the experience more pleasant is desirable.
“Minimally invasive knee replacement” is a term that is used by doctors, implant companies, and hospitals to refer to several procedures and strategies that you should understand carefully. Many of the so-called minimally invasive procedures are simply variations of existing techniques to implant total knees, except that they are done through smaller incisions. Other techniques are genuine advances that go much beyond just making a smaller skin cut. The ultimate goal is not only to make a shorter skin cut, but also to reduce deep muscle trauma associated with surgery, such that pain is lessened, discharge is expedited, and the need for prolonged physical therapy is reduced.
Partial Knee Replacement and Unispacer Surgery
When it comes to minimally invasive knee replacement surgery, you should be aware of two procedures that can be done instead of a complete knee replacement. One is called unicompartmental (or, partial) knee replacement, and the other is called a unispacer.
In partial knee replacement, only part of the knee joint is replaced. Usually, the inside of the knee (also called the medial side) wears out first, and in selected patients, replacing only this part of the knee (called the medial compartment) may be all that is needed. The procedure can also be done on the outside (or lateral portion) of the knee joint, and is often less frequently worn out than the inside, or the medial part of the knee joint.
Partial knee replacement uses small incisions and preserves the ligaments and other structures in the knee. Not surprisingly, the recovery is much faster, and the scar is smaller compared to a total knee replacement. However, few people meet the strict criteria for partial knee replacement. The surgeon has to be careful in selecting these patients; otherwise the partial knee replacement does not last, and requires another operation to convert it to a total knee replacement.
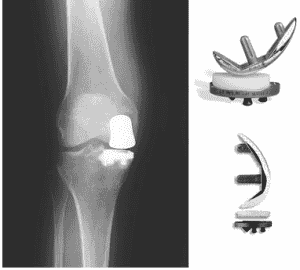
However, if the patient is a suitable candidate for a partial knee replacement, the results can be very durable for 10-15 years. Then, if necessary, a total knee replacement can still be done. Typically, fewer than 5 percent of patients with knee pain and arthritis will be appropriate candidates for this limited procedure. Figure 1 shows partial knee components and the front-to-back x-ray view of a knee with such a device implanted on the inside (or medial) compartment of the knee joint.
In unusual cases of knee arthritis, and in relatively young patients, a shim-like device called the unispacer might be appropriate. A unispacer is a device that is inserted in an arthritic knee only on the inside (or medial) compartment.
The unispacer acts like a spacer to separate the worn-out knee surfaces and keep them from grinding against each other. Compared to partial knee replacement procedures, even fewer patients will meet the criteria for a device such as the unispacer. Figure 2 shows a unispacer device, and a front-to-back x-ray of a patient who has had a successful unispacer on one knee, and a unicompartmental knee on the other. In this x-ray, the image showing the unispacer is on your left side, and the image showing the partial knee is to your right side.
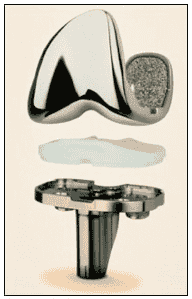
For the majority of patients with end-stage knee arthritis who have failed non-surgical methods of pain relief, a total knee replacement that addresses all the diseased cartilage is the most reliable and durable long-term option. Figure 3 shows the actual components used in a typical total knee replacement. The white polyethylene locks into the bottom piece, the tibial tray. The top part caps the prepared end of the femur bone. Actual movement of the artificial knee takes place between the top portion and the polyethylene layer.
Preparation for Surgery
Patient Knowledge and Awareness
Patient education is critical to ensuring a good outcome after a properly performed minimally invasive knee replacement surgery. Patient education means understanding information, and using knowledge to become an active, participating, and questioning partner in planning the procedure.
Awareness of realistic expectations, benefits, and limitations of knee replacement surgery are critical to a successful outcome after surgery. Every person recovers differently. Even two identical surgical procedures in the same person can be associated with a unique recovery. For example, patients who undergo two knee replacements at the same time, one on each knee, can experience somewhat different recoveries on each side.
What is Minimally Invasive Knee Replacement? You should know that the term “minimally invasive” is somewhat misleading, overused, and abused. Many hospitals, companies, and doctors will use the language of minimally invasive surgery as a marketing tool, often without understanding what the term means. A patient should be aware of this reality in today’s competitive health care environment.
The truth is that all surgery is invasive to the body and to the psyche. Surgery produces injury to the body. The response to surgery includes discomfort, altered emotions, side effects like nausea, altered appetite, constipation, and other unpredictable sensations. It takes time for the body and mind to heal. Other conditions such as diabetes, heart disease, and obesity can prolong recovery after any knee replacement operation. Minimally invasive surgery can reduce, but not eliminate, these normal physiological and psychological responses to surgical trauma.
Realize also that minimally invasive surgery does not mean risk-free surgery. All knee replacements, regardless of technique, have a small risk of infection, nerve injury, deep blood clots, premature implant loosening and failure, unexpected knee stiffness, continued pain, and unpredictable medical complications. No hospital, no doctor, no surgical technique in the world has reduced the risk of these adverse outcomes to zero. Complications are of course very rare, but patients planning knee replacement surgery should know about them, and take the time to understand them.
More about preparing for knee replacement surgery >>
Total Knee Replacement with a Shorter Incision
For many surgeons and hospitals, minimally invasive knee replacement amounts to doing the same operation through a smaller opening. In such cases, the procedure is the same beneath the skin; only the cosmetic appearance of the scar is smaller.
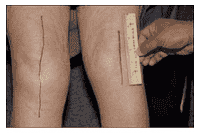
Figure 4 shows a standard total knee replacement scar on one side, and a minimally invasive total knee scar on the other side. Surgeons who perform at least 100 knee replacement procedures per year are in the best position to progressively begin shortening the incision, while keeping the procedure the same. The reason is that knee replacements through a smaller skin incision, keeping all else the same, requires more skill and training.
Minimally invasive knee replacements can be done by experienced surgeons using special instruments so that the incision length is reduced from the traditional 8-12 inches down to about 4 inches. Incision length ultimately depends on each patient’s severity of disease, anatomy, and amount of body fat. The more severe the arthritis and resultant deformity and the heavier the person, the longer the incision must be to allow surgery to be done safely. In most cases though, a 4-5 inch scar is sufficient for the surgeon to access the knee joint and to perform the procedure properly.
Many orthopedic implant companies have developed special instruments to assist in making shorter incisions, and conduct training seminars for surgeons. Learning more about the procedure by reviewing the patient educational materials provided on implant manufacturers web sites can be helpful. This also helps identify surgeons in your area who use a particular implant and are therefore qualified to safely perform the procedure.
Quadriceps-Sparing Total Knee Replacement
Beyond making the skin cut smaller, there are modern knee replacement procedures called “quadriceps-sparing knee replacements.” “Quadriceps” refers to four well- developed muscles in the front and sides of the thigh. These muscles combine just above the knee cap into a heavy tendon called the quadriceps tendon. The tendon controls the knee cap, and allows one to straighten out the bent knee, or do bench press exercises. This function is critical to normal walking, climbing stairs, and standing. Traditionally, knee replacement surgery involved cutting into the quadriceps tendon sufficiently to turn the kneecap over and push it out of the way to expose the arthritic joint during surgery. Most surgeons still do this, although they make the skin cut smaller in keeping up with modern times.
When surgeons refer to minimally invasive surgery of the “quadriceps sparing” type, the cut into the quadriceps tendon is much less so compared to the standard procedure. Also, the kneecap is not turned over; rather it is pushed over to the side during surgery. Special instruments allow this to happen through a smaller skin cut. Of the four quadriceps muscles, the insertion of at least three is preserved onto the knee cap this way, and only one (called the vastus medialis obliquus, or VMO) is surgically cut and later repaired. This so-called “quadriceps sparing total knee” is a legitimate minimally invasive procedure that improves recovery over the traditional approach described above, independent of the skin incision length. Discharge from the hospital in a day or two after surgery is possible in selected patients.
Sub-Vastus Total Knee Replacement
In the least invasive of any total knee procedure, even the VMO tendon is spared, i.e., not a single tendon on the knee cap is taken off. This newest minimally invasive knee replacement method is called the MIS-sub-vastus total knee approach. MIS stands for minimally invasive surgery. Sub-vastus means the surgeon goes below the VMO muscle and its tendon, instead of through it. The skin incision can be as small as 3-4 inches. None of the quadriceps tendon is disturbed; instead the muscle and tendon unit is lifted up and out of the way using special instruments that require expertise, training, and knowledge.
Very few surgeons are trained to do the sub-vastus procedure, and the outcomes are among the most favorable of all in knee replacement surgery. Using this approach greatly reduces the need for outpatient physical therapy in many total knee replacement patients.
The results of the MIS-sub-vastus method are dramatically superior, even when compared to knee replacements performed with any other technique, regardless of incision length. Patients complain of a lot less pain, and return to work faster. Also, the range of motion is restored quickly, often within a month from surgery.
Future Advances in Total Knee Replacements
On the horizon are more innovations, and each will be offered to patients as the safety and efficacy parameters are properly developed. The “lateral approach” is a minimally invasive knee replacement in which the entire operation is done by making the skin cut on the outside of the knee. The kneecap and the muscles supporting it are disturbed even less than during any of the procedures above. This is because most of the muscles are in the front and the inside of the knee joint, while the lateral approach is from the outside of the knee. The upside is even faster recovery with less pain and virtually instant control over the leg muscles by the patient after surgery.
Computerized navigation allows surgeons to place knee components with more accuracy. This increased accuracy is critical to the long-term functioning of the artificial knee. Navigational technology to guide the implantation of knee components, with the latest generation of electromagnetic probes that deliver positional data from the bones to software, enables precise alignment of the limb in real time.
Finally, knee replacement components are being fundamentally redesigned to address specific areas of the knee that are prone to arthritis. In the future, these components will be inserted through ever smaller incisions, with no muscle trauma, and using robotics and computer navigation for implantation. Yet further in the horizon is the promise of stem cell research and creating layers of natural cartilage individualized to each patient so that the nature of knee replacement surgery is changed radically.
More about the advantages of minimally invasive knee replacement surgery >>
During the Procedure
During minimally invasive knee replacement surgery, you lie on your back. Usually, a spinal anesthetic with sedation is sufficient. The procedure takes anywhere from 30-45 minutes to complete. The instruments used to approach the knee joint are specially designed by the implant companies to facilitate the use of small exposures.
The use of computer navigation is an important advancement that may contribute to the overall safety and efficacy of any knee replacement procedure. Computers can improve the ability of the surgeon to accurately align and orient the prosthetic components. In nearly all knee replacements, the surgeon must place metal rods inside the hollow parts of the major bones close to the knee joint (that is, the femur and the tibia). This step is needed for the surgeon to measure knee alignment, and to place the implants accurately. However, the risks of pushing metal alignment rods into bone include disruption of the bone marrow, bleeding, and an increased incidence of blood clots.
Computer navigation is superior in its ability to help your surgeon consistently align and position the parts of the knee implant and it does so without invading the cavities of any of the long bones around the knee joint. This technology represents the future of knee replacement surgery. Small markers are placed at vital anatomical points on the leg, and the computer-based system can read the positions of these markers, compute the optimal alignment, and customize it for each patient. Ultimately, all knee replacements will likely be performed using some method of software-enabled navigation.
After the Procedure
Many surgeons combine small incision knee surgery with other methods to relieve pain and to facilitate recovery. For example, spinal and epidural anesthesia can speed up recovery. Newer anesthetic agents can reduce the incidence of nausea and confusion associated with older drugs. Non-narcotic pain relievers and injections of painkillers into the tissues during the surgery make for a more pleasant experience afterwards.
With modern knee replacement techniques, you are encouraged to become mobile much earlier than with the standard method of knee replacement. Many people are encouraged to get out of bed either the same day or the next day, with the help of a physical therapist.
Pain pumps that infuse painkillers into the incision, patient-controlled analgesics, and newer anti-inflammatory drugs may all be used in combination to speed up recovery.
Even though modern surgery can facilitate recovery and reduce the risk of blood clots, minimally invasive procedures cannot eliminate the risk of a clot. Some method of reducing the likelihood of blood clots after surgery is still necessary, regardless of how small an incision your surgeon used to replace your knee. Surgeons may use a combination of methods to reduce the risk of blood clots.
More about recovering from knee replacement surgery >>
Next Steps
If you are contemplating knee replacement surgery, the first resource is asking friends or relative who have had a similar procedure about their experience. This may help you in choosing a hospital and a doctor.
Another useful resource is to get in touch with a joint replacement surgeon at your local teaching hospital or university medical center. Many joint replacement surgeons in academic medical centers welcome email communications from patients, even if the patient lives far away. It makes sense to get a second opinion this way, because most minimally invasive joint replacement operations are first developed and tested in medical schools and research institutions.
Regardless of their talent, reputation, or skill, private practice surgeons cannot match the resources or extent of exposure available at university-based hospitals when it comes to new surgical techniques. Community surgeons may be under pressure to adopt and advertise minimally invasive surgery. As explained in this article, all minimally invasive knee replacement surgery is not the same; and to get the optimal benefit of such a procedure requires the application of several complex techniques and modalities.
Ask if your doctor has a web site, and if email communication is welcomed. Review the web site so that you can refine your questions and concerns for your visit. Face time with a doctor is often at a premium, so that such preparation can help you maximize the utility of the appointment. Make sure you check the credentials of your doctor, often these will be posted on the web site if your doctor has this resource. Your chemistry and comfort level with your surgeon are important since joint replacement surgery is not a short-term undertaking. Your doctor should not only encourage questions, but also encourage the use of email and other resources to facilitate direct communications.
More on deciding about hip replacement surgery >>
The Risks of Minimally Invasive Knee Replacement Surgery
Minimally invasive surgery is still an invasive surgical intervention, with all the considerations and cautions inherent to any trauma to the body. Small incisions are known to have complications of their own, particularly when performed by surgeons who are not experienced with the newer techniques. Because of limited surgical exposure, problems such as improper placement of components, nerve injury, fractures during the procedure, and a longer duration of surgery are possible. Be sure to ask your doctor about such complications, as they are documented in peer-reviewed literature. If your doctor does not address these concerns or if your doctor is unaware of the complications, seek a different doctor.
The general complications of any joint replacement still apply to minimally invasive knee replacement surgery. These risks include blood loss, the possibility of blood clots or infection after surgery, and the need to follow certain precautions to adjust to a lifestyle with a prosthetic device. Unrealistic expectations, a lack of information and preparation, and a failure to become an active and aware participant in the surgical process can lead to disappointment after minimally invasive knee replacement.
Also, keep in mind that different people react differently to the same procedure, depending on their body weight, associated medical conditions, family support, cultural background, psychosocial influences, and other unpredictable factors. Minimally invasive or not, please embark on any knee replacement surgery only after taking a keep pause, educating yourself, and thinking over these considerations carefully and deliberately.
Results
The long-term results of minimally invasive knee replacement surgery are not currently known but will be published as surgeons gain more experience with these techniques. If the knee implants are placed properly, and if the surgeon pays attention to the details inherent in the placement of artificial devices in the skeleton, the new knee should last through several decades of reasonable use.
The short-term results of minimally invasive knee replacements are favorable in terms of an earlier discharge from the hospital, less pain, and a faster return to day-to-day activities. The need for physical therapy following surgery is minimized by techniques that reduce trauma to the skin, muscles, and tendons. The complications reported by some studies describing the early results of minimally invasive knee replacement are inherent in any new procedure. This is why surgeon selection, surgeon experience, and patient education are so important when it comes to surgical techniques.
When to Seek Medical Care
Minimally invasive knee replacement surgery does not change the reasons for seeking a knee replacement in the first place. You should postpone knee replacement as long as possible. Knee replacement surgery should be sought only for debilitating pain that is not responding to pain medications, exercise, weight loss, and reasonable activity modification. Regardless of the surgical technique, all knee replacements are salvage operations for worn-out knees that can no longer do their job. No artificial knee, regardless of how expertly it is implanted, can ever be a perfect substitute for the real knee. Knee replacement surgery involves some lifestyle alterations and certain considerations that apply to any artificial implant.
The golden rule is that elective surgery, such as a knee replacement, should be avoided until all other reasonable treatment options have failed. Not only do newer technologies keep evolving over time, but also it is best for you to get as much use out of your own joints as possible. The risk of surgery should be postponed until all non-surgical options have been exhausted.
Contributors
- University of Missouri Medical School department of Orthopedic Surgery provided full text for publication on BoneSmart.org
image credit: National University Hospital
Filed Under: Knee ReplacementKnee Replacement, Resurfacing, Revision